Popular
How to Build the Perfect Oral Care Routine in 2025
Jul 30
Why Your Gums Bleed and How to Fix It Fast in 2025
Jul 30
Top 5 Oral Care Mistakes and How BrushO Fixes Them
Jul 29
What Makes a Toothbrush “Smart”?
Jul 22
BrushO Smart Toothbrush: Gentle, Powerful, Travel-Friendly
Jul 19
BrushO: The Future of Smart Oral Care—Redefining the Way You Brush
Jul 17
Atrás
How a Blocked Nose Can Quietly Affect Your Oral Health-11120m ago
-11120m ago
A blocked nose is commonly dismissed as a minor inconvenience, yet persistent nasal obstruction can reshape oral health in subtle but measurable ways. When nasal airflow is compromised, the body compensates with mouth breathing — especially during sleep — altering saliva balance, microbial ecology, jaw posture, and gum resilience. Reduced salivary protection increases plaque accumulation, enamel vulnerability, and inflammation risk even in individuals who maintain regular brushing routines. Understanding this overlooked connection enables proactive prevention. This article explores the physiological mechanisms linking nasal blockage and oral health decline, identifies early warning indicators, and outlines science-backed strategies to maintain oral stability — including precision-guided brushing supported by AI-powered tools like BrushO.

How Nasal Blockage Changes the Oral Environment
Nasal breathing plays an essential physiological role beyond respiration — it regulates humidity, filters particles, and maintains proper oral posture. When airflow is obstructed due to allergies, infection, congestion, or anatomical variation, breathing shifts toward the mouth.
Chronic mouth breathing alters oral function in several key ways:
• Accelerates moisture loss from oral tissues
• Reduces salivary buffering capacity
• Increases oxygen exposure for bacterial growth
• Changes resting jaw and tongue positioning
These shifts create a microenvironment more conducive to plaque accumulation and gum irritation, even before symptoms appear.
Saliva: The Silent Defender That Gets Compromised
Saliva is central to oral ecosystem stability. It:
• Neutralizes acid produced by oral bacteria
• Remineralizes enamel with calcium and phosphate
• Removes food particles
• Regulates microbial populations
Mouth breathing reduces saliva retention, producing subclinical dry mouth — dryness that may not feel severe but still affects protective function.
Consequences may include:
• Faster plaque formation
• Increased bacterial volatility (odor compounds)
• Higher enamel demineralization risk
• Reduced gum tissue resilience
Because adaptation occurs gradually, many individuals fail to recognize this degradation.
Night-Time Amplification of Risk
The most pronounced oral effects occur during sleep. Physiologically:
• Saliva production decreases at night
• Mouth breathing accelerates evaporation
• Bacterial activity continues uninterrupted
This combination allows extended microbial activity across tooth surfaces and gum margins.
Morning indicators may include:
• Persistent halitosis
• Sticky biofilm sensation
• Localized gum tenderness
• Jaw stiffness or fatigue
These signs represent ecological stress rather than isolated hygiene failure.
Postural Effects: Tongue, Jaw, and Bite Mechanics
Breathing mechanics influence craniofacial posture. Nasal obstruction encourages:
• Lower tongue resting position
• Open-mouth jaw alignment
• Altered occlusal balance
Long-term outcomes may involve:
• Uneven tooth wear patterns
• Jaw tension or clenching
• Bite instability
In developmental stages, chronic mouth breathing can influence facial growth patterns. In adults, structural change is subtler but still biomechanically relevant.
Gum Health Vulnerability in Mouth Breathers
Dry airflow across the gingival tissue reduces lubrication and increases exposure to irritants. Clinical observations associate mouth breathing with:
• Gingival redness
• Swelling
• Bleeding during brushing
• Higher gingivitis prevalence
Importantly, this inflammation may persist despite regular brushing if coverage along the gumline is inconsistent.
Preventive Strategies When Nasal Blockage Persists
Addressing the root respiratory cause should remain the priority (allergy management, airway evaluation, sleep positioning). However, oral resilience can be strengthened through targeted hygiene:
• Prioritizing full plaque removal
• Cleaning along gum margins
• Avoiding aggressive brushing pressure
• Maintaining hydration
• Monitoring early inflammation signals
Consistency and technique precision become particularly important under elevated oral stress conditions.
Why This Connection Is Frequently Overlooked
The nasal–oral relationship lacks dramatic symptoms. Instead:
• Damage accumulates slowly
• Pain rarely appears early
• Changes are ecological rather than acute
Because cause and effect unfold gradually, nasal obstruction remains an underestimated contributor to oral instability.
Supporting Oral Stability with Precision Brushing
When breathing patterns elevate risk factors, improving brushing accuracy helps maintain equilibrium. BrushO supports this by:
• Guiding coverage across all zones
• Reducing missed gumline areas
• Monitoring pressure consistency
• Reinforcing routine stability
These features help compensate for environmental stressors by ensuring plaque removal remains thorough and balanced.
A blocked nose can quietly reshape oral health through moisture loss, microbial shifts, and biomechanical changes. While the effects are gradual, they are measurable and preventable. Recognizing breathing patterns as part of oral wellness allows earlier intervention and better long-term outcomes. Combining airway awareness with consistent, precision-driven oral care ensures resilience — even when physiological conditions are less than ideal.
Early Signs Your Teeth Are Starting to Decline
-12670m ago
Can You Safely Delay Dental Visits Without Harming Your Teeth?
-10150m ago
Popular
How to Build the Perfect Oral Care Routine in 2025
Jul 30
Why Your Gums Bleed and How to Fix It Fast in 2025
Jul 30
Top 5 Oral Care Mistakes and How BrushO Fixes Them
Jul 29
What Makes a Toothbrush “Smart”?
Jul 22
BrushO Smart Toothbrush: Gentle, Powerful, Travel-Friendly
Jul 19
BrushO: The Future of Smart Oral Care—Redefining the Way You Brush
Jul 17
Publicaciones recientes
Why Your Saliva Flow Changes Throughout the Day
Saliva flow fluctuates throughout the day due to circadian rhythm, hydration, diet, and stress. Learn why it matters for oral health and how smart brushing protects teeth during low-saliva periods.
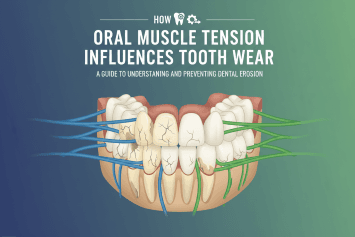
How Oral Muscle Tension Influences Tooth Wear
Oral muscle tension and jaw strain can accelerate tooth wear, enamel erosion, and gum stress. Learn how muscle habits influence dental health and how smart brushing supports long-term protection.
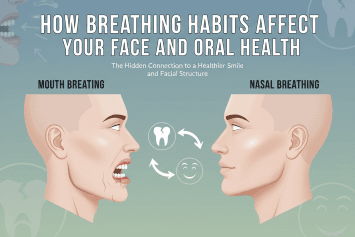
How Breathing Habits Affect Your Face And Oral Health
Discover how mouth vs nose breathing affects oral health, facial development, jaw alignment, and sleep quality — and how to protect your teeth and gums with proper habits.
Brushing More Than Twice a Day Is Helpful or Harmful?
Is brushing more than twice daily good for your teeth? Learn how brushing frequency affects enamel, gums, and sensitivity, and discover dentist-backed guidance for safe oral care habits.
What Does Eating Sugar at Midnight Do to Your Mouth?
Discover how eating sugar at midnight affects oral bacteria, enamel health, and overall wellness. Learn why late-night snacking raises cavity risk and how proper brushing protects your teeth.
How Brushing Confidence Shapes Oral Health Outcomes
Discover how brushing confidence influences oral health outcomes, plaque control, and gum protection. Learn why self-efficacy in brushing technique matters and how smart toothbrush feedback improves long-term dental health.
Why Inconsistent Sleep Schedules Harm Gum Recovery
Irregular sleep schedules can slow gum recovery, worsen inflammation, and disrupt oral microbiome balance. Learn how sleep affects periodontal health and how smart brushing habits help protect your gums.

Why People With the Same Brush Get Very Different Results
Discover why two people using the same toothbrush can experience different oral health results. Learn how technique, pressure, coverage, and AI-guided brushing influence outcomes.
How Habit Loops Control Your Oral Health
Learn how habit loops shape your oral health and brushing consistency. Discover the neuroscience behind oral hygiene routines and how AI-guided tools like BrushO strengthen healthy dental behaviors.
Why Your Brain Fights Against Good Brushing Habits
Discover why your brain resists consistent brushing habits and how behavioral science, habit formation, and AI-guided tools like BrushO can improve oral hygiene consistency.
